
A WIRELESS VOICE/DATA COMMUNICATION SYSTEM
IN A LARGE HOSPITAL
Eisuke Hanada
Department of Medical Informatics, Shimane University hospital, Izumo, 693-8501, Japan
Takato Kudou
Department of Electric and Electronic Engineering, Faculty of Engineering, Oita University, Oita, 870-1192, Japan
Keywords: Wireless communication, Cellular phone, PHS, wireless LAN, information security
Abstract: Computer systems, often called hospital information systems (HIS), have been installed in most large
Japanese hospitals for administration of the basic medical information of patients, for making entries on
medical charts, and for prescribing medication. In almost all cases, HIS have a server/client type structure,
with the servers and client terminals connected with a LAN. For voice communication among the hospital
staff, a landline telephone is often used. Fixed-line call systems (nurse call systems) are used for
communication between patients and nurses. The potential demand for the introduction of wireless
communication devices for data/voice communication into hospitals is high because of the promise of
savings these technologies bring by improving patient service and labour efficiency. However, because of
guidelines made to reduce problems that might be caused by electromagnetic interference (EMI) with
medical electric devices and administrative fears about potential problems, the introduction of these systems
has, until recently, been shelved in almost all cases. Because in recent years it has became possible to
control the electromagnetic waves emitted by mobile communications apparatus and to protect against the
possible occurrence of EMI, the number of hospitals introducing such wireless communication has grown.
We report a case of a university hospital in which data and voice wireless communication have been safely
and efficiently introduced
1 INTRODUCTION
Computer system installation is progressing rapidly
in Japanese hospitals. Computer systems designed
for storing the basic medical information of patients,
for making entries on medical charts, for
information retrieval, and for the prescription of
medication have been installed in most hospitals
with 600 or more sickbeds. Usually called a hospital
information system (HIS), most have a server and
client type structure. Many types of systems exist in
which servers located in a special hospital server
room communicate with client terminals in
consultation rooms or nurse stations by way of a
LAN using TCP/IP.
Voice communication among hospital staff
members, however, is often still done with fixed,
landline telephones. A fixed-line call system is
usually used for communication between a patient
and a nurse in which the patient pushes a button on
the sickbed and a lamp on the indicator panel in a
nurse station lights up. An intercom may also be
used by which a nurse can talk with the patient who
pushed the button. This system is usually called a
"nurse call system."
The potential demand for the introduction of
wireless communication devices for data/voice
communication into hospitals is high because of the
promise of savings these technologies bring for
improving patient service and labour efficiency
(Nelson, 1999). However, because of reports since
1993 of problems caused by electromagnetic
interference (EMI) with medical electric devices and
guidelines enacted in many countries to protect
against such interference, the introduction of such
systems has been shelved in almost all hospitals.
124
Hanada E. and Kudou T. (2005).
A WIRELESS VOICE/DATA COMMUNICATION SYSTEM IN A LARGE HOSPITAL.
In Proceedings of the Second International Conference on e-Business and Telecommunication Networks, pages 125-130
DOI: 10.5220/0001413101250130
Copyright
c
SciTePress
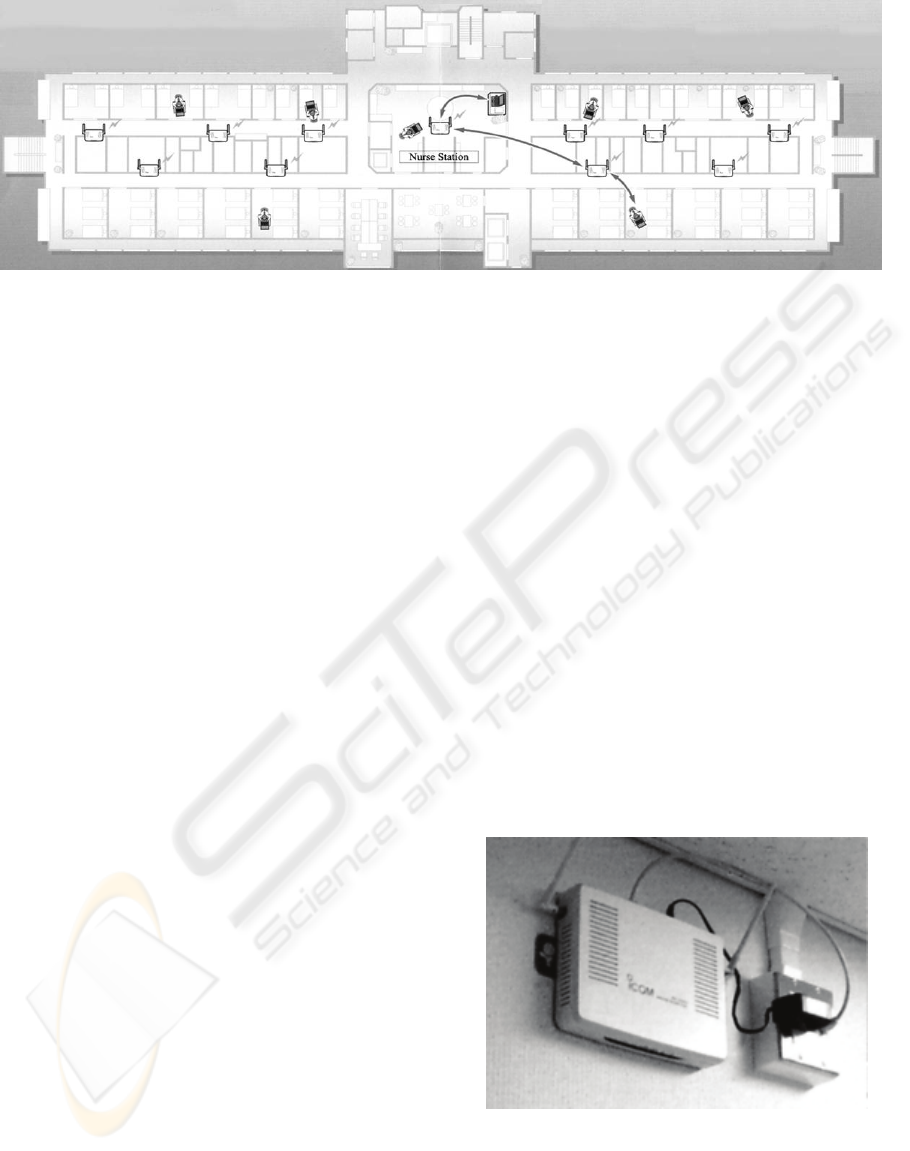
Fi
g
ure 2: AP-5100 in a ward corrido
r
Since in recent years it has became possible to
control the electromagnetic waves emitted by mobile
communications apparatus and to protect against the
possible occurrence of EMI, the number of hospitals
introducing such wireless communications has
grown. In this paper, we report a case of a university
hospital in which wireless communication have been
safely and efficiently introduced. (hereafter termed
the target university hospital). The target university
hospital is described in section 2.1. Wireless data
communication is reported in section 2.2, followed
by wireless voice communication for staff and
patients in section 2.3. Finally, the needs and
effectiveness of in hospital wireless communication
are discussed.
2 INTRODUCTION OF
WIRELESS COMMUNICATION
IN A UNIVERSITY HOSPITAL
2.1 Outline of the target university
hospital
The target university hospital is located in western
Japan, has 21 specialised departments, 616 beds, and
about 300 doctors and 350 nurses. The target
university hospital has one ward building with 12
wards of about 50 beds each, an ICU and an NICU.
A special ward is only for children and another is
only for psychiatric patients. Also, one ward is
designated for women only. Although there are
some private rooms, most accommodate from 2-6
persons. Each ward has eight to ten daytime and two
or three night nurses. A minimum of one doctor is
required to be stationed at each ward at all times to
perform required medical treatment, but usually
more than one is on duty
2.2 HIS wireless data
communication
The HIS of the target university hospital consists of
44 servers and 512 client terminals. Of these, 60
client terminals are connected with servers using
wireless LAN. These terminals are limited to use in
the wards by the medical staff. The specification of
the adopted wireless LAN is IEEE802.11a for the
following reasons.
Apparatus that emit electromagnetic waves in the
2.45GHz band, such as heaters, and microwave
ovens, are often found in hospital wards. The data
transfer rate is higher than that using IEEE802.11b
and 11g.
Eleven access points are located in each floor, as
shown in Fig.1. For the access point, we adopted the
AP-5100 (ICOM Inc., Fig. 2).
Because the security of personal information
important, to prevent electric wave interception the
SSID value is changed on each floor and connection
attempts using the “Any” setting of the SSID are
refused.
Figure 1: An image of the location of access points in one floo
r
A WIRELESS VOICE/DATA COMMUNICATION SYSTEM IN A LARGE HOSPITAL
125

Figure 3: A PHS terminal used in the
target university hospital
The AP-5100 has adopted OCB AES (128 bits)
as a cipher system, and high-speed encryption and
decryption are possible. Also, a connectable Media
Access Control (MAC) address can be registered
into each access point. Therefore, if PCs other than
terminals permitted to be connected are used in any
ward, they cannot be connected to the hospital LAN.
Furthermore, to prevent unauthorised entry into the
HIS, authentication with ID and a password is has
been added and all communications are logged.
In addition to uploading and input of patient
information at bedside, patient checks using barcode
scanning and review of medical treatment charts can
be done on this system. Not only is medical
efficiency improved, but the system also protects
against input failures and input mistakes by
eliminating the need to move from bedside to the
fixed terminals in the nurse station. Also, because
reference to required medical information is possible
at the bedside, it is also useful from the aspect of
improvements in the safety of medical treatment.
Moreover, messages and directions previously were
written on memorandum pads and passed by hand
among the staff, resulting in personal information
being seen by many people. The protection of
personal information is improved through the use of
this system.
2.3 Mobile voice communication
2.3.1 Mobile voice communications between
staff members
In the target university hospital, both landline
telephones and the Personal Handy-phone System
(PHS) are used for voice communication between
staff members. PHS is a totally digital mobile
communication system with low output power
(Hanada, 2000) developed in Japan, and its use is
spreading in China and Southeast Asian countries.
The frequency of the electromagnetic signal used by
PHS is in the 1.9GHz band, and the output of a
terminal is a maximum of 80mW. When the distance
from a base station to a terminal is about 100m, the
output of the base station can be reduced to as low as
160mW. Almost no EMI with medical electric
devices by the electromagnetic signals emitted by a
PHS terminal was found in investigations by EMCC
of Japan (EMCC, 1997) and the Ministry of Public
Management, Home Affairs, Posts and
Telecommunications of Japan (MPHPT, 2002).
In many large Japanese hospitals, not only in
university hospitals, nurses using PHS instead of the
traditional nurse call system terminal can respond to
calls from patients immediately, even when out of
the nurse station, thus increasing efficiency,
improving patient service, and raising the level of
medical safety.
Besides this, doctors working in the target
university hospital have access to a public PHS
terminal (WILLCOM, Inc., Fig.3), the cost effective
“Anshin-da-phone” service with limited functions.
In this system, calls can be received freely, but a
limit is set at three numbers, designated by the
subscriber, that can be called. As seen in Figure 3, a
red strap is connected to the PHS terminal to serve
notice that the terminal has been registered for use in
the hospital. The use of PHS makes it unnecessary
for nurses and pharmacists to physically search for a
doctor, and makes it possible to quickly ask
questions and receive the necessary feedback.
To determine the effectiveness of the PHS
system for doctors, the number of calls received on a
fixed-line telephone in a ward was compared for one
week before and after the introduction of PHS.
Results are shown in Table 1.
Table 1: Number of calls received on weekdays (5 days)
before and after the introduction of PHS
Section
Calls before
introduction
Calls after
introduction
Wards 1216 588
Visitor sections 458 356
Other sections 116 212
Total 1790 1126
As shown in Table 1, the total number of calls
received at wards was reduced by more than half.
However, the number of calls received at the other
sections increased, possibly because even though
PHS emits a safe level of electromagnetic signals,
carrying such phones into surgical rooms is
forbidden.
ICETE 2005 - WIRELESS COMMUNICATION SYSTEMS AND NETWORKS
126

2.3.2 Mobile communication as a service for
patients
The target university hospital permits the use of
cellular phones by outpatients, inpatients, and
visitors to unrestricted zones. In Japan, 85,500,000
or more cellular phones are now in use, with 75% or
more people having a cellular phone (TCA, 2004).
Many people have become so dependant on them
that a syndrome called "cellular-phone dependence"
has been coined for people who cannot live without
them. Also, the use of cellular phones in business is
widely promoted as they are now recognised as
being indispensable for doing business. Due partly
to the above factors, the demand for communication
using cellular phones by both outpatients and
inpatients is growing. Especially for inpatients, the
free use of a phone can decrease stress and the sense
of isolation caused by hospitalisation, thus raising
the Quality of Hospital Life (QOL). Other factors
may account for some of the increased demand for
cellular-phone use. For example, no reports of
malfunction of medical devices have been seen in
recent years. The third generation mobile phone
systems, which reduced the electric wave output
have become popular. Also, medical devices have
improved protection against electromagnetic waves.
The target university hospital defined criteria for
cellular phone use, with reference to experimental
results (EMCC, 1997, Hanada, 2000, MPHPT, 2002)
as shown in Table 2, and permitted the use of
cellular phones in limited areas from January, 2004.
Table 2: Conditions for cellular-phone use in the target
university hospital
• Cellular phones can be used only in a visitor lobby, a
single bed sickroom, and in dining rooms.
• The medical staff can use cellular phones at nurse
stations and in conference rooms
• Cellular phone use is not allowed within 50cm of
medical devices
• Patients connected to medical devices are prohibited
from using cellular phones
• After a set time for turning out sickroom lights, the use
of cellular phones is prohibited
• Staff members are not allowed to use a cellular phone
during rounds, while walking, or during explanations
to patients or their family.
In the target university hospital, these rules are
widely displayed and are specified in the hospital
guidelines. The co-operation of patients and staff
members has been requested, and no interference
with medical devices has been observed since these
rules were put in effect.
3 DISCUSSION
In Japan, other than the target university hospital
there are no hospitals with more than 600 beds using
wireless communications for both data and voice
communication. This is because restriction of
cellular phone use is economically cheaper and
responsibility can be avoided by hospital
administrators who fear EMI and who do not want to
take the measures necessary to mitigate against EMI.
However, by keeping cellular phones away from
medical devices and by using mobile phones or
wireless LAN apparatus with weak electromagnetic
wave output, it is possible to stop or minimise EMI
with medical devices, as shown by previous
experimental results (Hanada, 2000, Hanada, 2004).
In Japanese hospitals, long periods of time spent
in treatment as an outpatient has been a big problem.
Also, inpatients have, in many cases, been restricted
from communicating with persons outside the
hospital. The dissatisfaction of both groups has
grown. Recently, the Japan Council for Quality
Health Care (JCQHC) has been asked for a ruling
about cellular-phone use in hospitals. The JCQHC
has made standards and checks hospitals for
compliance. Japanese hospitals that have been
checked for evaluation of clinical function have felt
the evaluations were fair. The newest version of the
JCQHC standards require that a space be designated
in which cellular phone use is permitted or that an
alternative communication means be in place if the
institution wishes to meet the evaluation standards
(JCQHC, 2005). Such evaluation is not mandatory,
but permission for cellular-phone use taking into
account these factors has resulted in improvements
in service to patients.
Before mobile communications systems were
installed in Japanese hospitals, many telephone calls
searching for doctors were placed, which took quite
a lot of time. Because secretaries and office
personnel are seldom hired to work in wards in
Japanese hospitals, there are many cases in which
nurses receive calls that require administrative work,
reducing their ability to complete their nursing
responsibilities. For example, when a pharmacist in
the pharmacy has a question about a prescription, it
is necessary to contact the doctor concerned for
confirmation of the prescription and correction, if
necessary. However, in large hospitals, because the
pharmacists in many cases work in places distant
from doctors, the pharmacists do not have the means
to know the current location of each doctor.
Therefore, they had to call various wards or
consultation rooms.
A WIRELESS VOICE/DATA COMMUNICATION SYSTEM IN A LARGE HOSPITAL
127

Doctors working in Japanese university hospitals
in the past, in many cases, received emergency calls
through a pager. However, a pager has only a
message receiving function and can not place calls,
and the caller can not know whether the doctor has
read the message. Therefore, they are not suitable
for communications that require immediate reply.
This is the same with communications using E-mail.
Furthermore, public pager service in Japan will be
stopped within the next year.
Installing wireless communication will result in
fore timely communication, which will result in
significantly improved medical safety. For example,
when a pharmacist has a question concerning a
prescription, drugs can not be given to the patient
until the question has been answered. Also, the
immediate communication gives nurses more time
for providing direct nursing care. This results in
fewer patient accidents and quicker response times
when patients have a sudden change in their disease
course.
Unrestricted mobile voice communication not
only may become the cause of EMI but may cause
conflict due to the noise generated by a telephone
call or may result in medical accidents due to a lack
of attentiveness. Therefore, limiting the areas in
which phones are allowed is important for the
purpose of preventing EMI, controlling noise, and
preventing medical accidents (Hanada, 2005).
In Japan, some hospitals do not have wireless
communication, but place a computer that serves as
a joint use terminal for business use and for patient
service at each bed. However, when taking into
account other factors, such as multi-patient
sickrooms, the fact that some patients are not
notified of their precise diagnosis, that the user
authentication of these systems depends only on an
ID and a password, and that the cost of installing a
terminal at each bed is extremely high, these systems
may not be viable. Other methods of providing
Internet terminals as a patient service may be better
from the standpoints of both economics and patient
privacy.
To prevent the leakage of personal and hospital
information, it is necessary to take all possible
physical means available, but user education,
especially the education of the medical staff, is the
most important aspect.
4 CONCLUSION
A system for wireless voice/data communication in a
university hospital was shown. In many hospitals,
wireless communications have not been introduced
for fear of the possibility of EMI. Aimed at realising
the benefits of cost efficient information sharing and
instant communication while insuring medical
safety, wireless data transmission and mobile voice
communication with low output power systems will
be widely used in the future as they become
evermore efficient, useful, and safe in the medical
environment.
ACKNOWLEDGEMENT
The authors wish to thank the following companies
that offered data and information: CARECOM Co.,
ltd., ICOM Inc., and WILLCOM, Inc. This study
was partially supported by grants-in-aid from the
Japan Society for the Promotion of Science
(No.17390152).
REFERENCES
EMCC, 1997. Research report of the usage of radio-
communication equipment such as cellular telephones
(in Japanese). Proc. Electromagnetic Compatibility
Conference (Japan). Tokyo, Japan
Hanada, E., 2000. Electromagnetic interference on
medical equipment by low power mobile
telecommunication system. IEEE Transactions on
Electromagnetic Compatibility vol.42 (4) pp.470-476
Hanada, E., 2004. A Pilot Study on Electromagnetic
Interference between Radio Waves Used in Wireless
LAN Communication and Medical Electronic
Equipment. Journal of Information Technology in
Healthcare vol.2 (4) pp.281-291
Hanada, E.,
2005.
Safe Use of Mobile Telecommunication
Systems for Clinical Communication and Data
Collection. Proc. First International Conference on
Complex Medical Engineering - EMC2005 pp.377-
381
JCQHC, 2005. Self-valuation sheet for assessment (for
general hospitals) (in Japanese). Japan Council for
Quality Health Care, Tokyo, Japan
MPHPT (Ministry of Public Management, Home Affairs,
Posts and Telecommunications, Japan), 2002. Results
of investigation into the effect of electromagnetic
waves on medical equipment. In their Web page,
(http://www.soumu.go.jp/joho_tsusin/eng/Releases/Te
lecommunications/news020702_1.html)
Nelson, L., 1999. Step-by-step Guide to Selecting Mobile
Wireless Devices. Nursing Management pp.12-13
TCA, 2004. “Number of subscribers by Carriers (as of
December 31, 2004) Telecommunications Carriers
Association,” In their Web page
(http://www.tca.or.jp/eng/database/daisu/yymm/0412
matu.html)
ICETE 2005 - WIRELESS COMMUNICATION SYSTEMS AND NETWORKS
128
